At our annual Regenexx network provider conference in Denver this past week, a network physician who is more focused on interventional spine came up and thanked me for introducing him to a new treatment for neck pain – platelet lysate. This one change had revolutionized his practice as he found it much more effective than injecting steroids into the epidural space. This reminded me of a review left on Facebook a few weeks ago by a patient who agreed that platelet lysate had also changed her life.
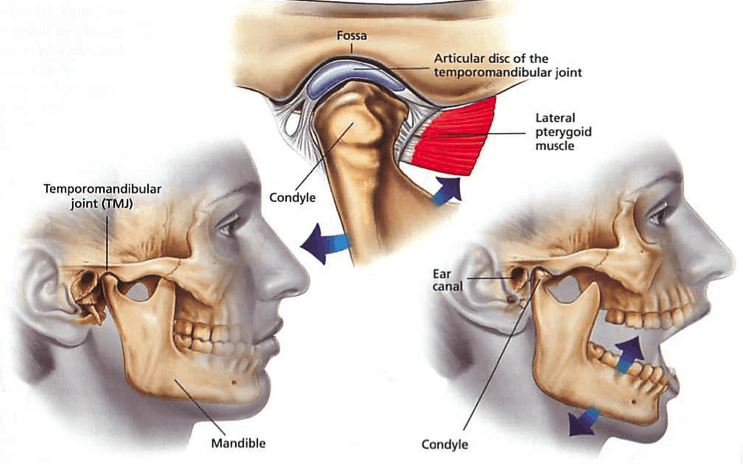
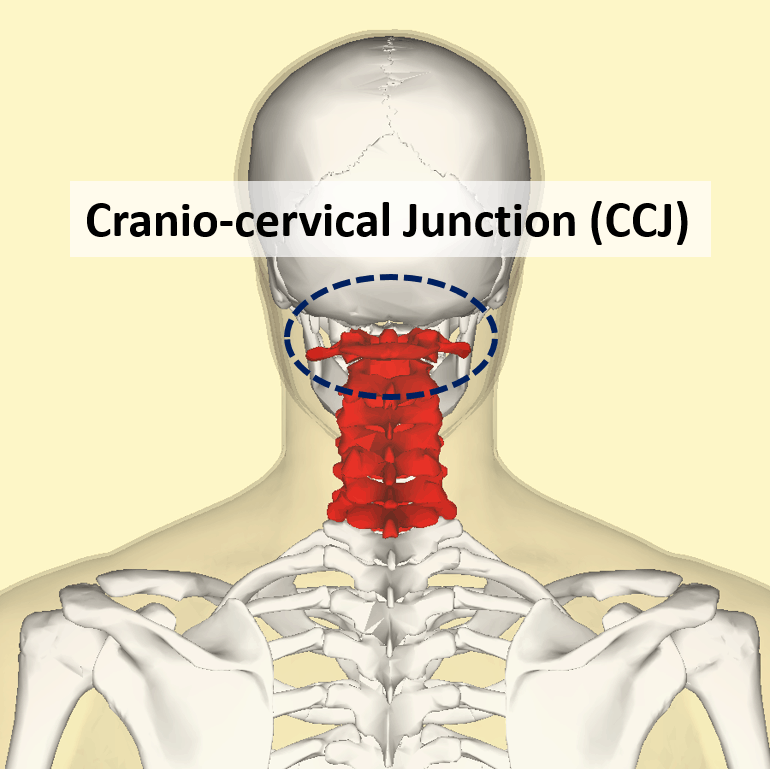
We’ve always done many things in regenerative orthopedics that that nobody else does. One of those things is isolating the growth factors present in platelet rich plasma and using those as a potent natural anti-inflammatory to replace the harmful effects of epidural steroid injections (ESI). The latter shot is used to help reduce swelling around irritated nerve roots, but can also have serious side effects like the destruction of bone and osteoporosis in middle aged and older women. By using this growth factor cocktail instead of steroids, not only can we get rid of inflammation around nerves and the side effects, but we also believe that we can improve the blood supply around compressed nerves.
Heidi’s journey as described in her post below is consistent with our experience of just how well platelets can work for patients. In her case it took awhile to latch onto the right injection route, but we got here there in the end!
“I had a sporting accident in 2006 and resulting C6 C7 fusion at the Mayo Clinic in 2008. Surgery and healing were as expected with no major complications except for the nature of my specific body. The post-surgical period was extremely painful and it took me a year to heal with the help of a bone growth stimulator. I lost two jobs because I could not maintain the required pace. Unfortunately, my adjacent cervical discs did not like the change. After exploring all options, including additional surgery, I began treatment with Dr. Centeno/Dr. Schultz in late 2012. At that time, I could not be upright after 3 PM. My life was severely limited. I could not exercise or work. My social life was over. The initial facet platelet lysate injection and two prolotherapy treatments did not help. (Spines can be notoriously difficult to pinpoint the cause of the pain). Mark Riley’s PT was wonderful. They had me wean off all narcotics, NSAIDS, a statin and baby aspirin (my PCP did not agree with eliminating the statin and the baby aspirin. It is challenging to reconcile differing advice from doctors involved in your care. At some point, you just have to pick the condition that is most important to your quality of life and go with that Doc) After about nine months of trial and error, a C5 C6 epidural platelet lysate injection in September 2013 gave me my life back. I now experience very little pain and only when extremely fatigued. My last injection was with Dr. Schultz a year ago. I had two injections in 2013 and two in 2014. I have not had an injection yet this year. I am starting to have a bit more pain and may have one before the end of 2015. Time will tell. For me, $500 per injection is a small price to pay for a life largely free of chronic, severe pain…These doctors are the real deal. They are on the cutting edge of medical innovation and treatment advances. The pain management doctor who treated me for five years with traditional narcotics and steroid injections was having them treat his knee. All of my second opinions from various practitioners, except surgeons, said this is clearly the future of orthopedics. I am a person who does her homework. Do not let anyone cut into your body without first exploring the possibility of a regenerative treatment for your condition. There may always be a place for surgery and artificial joints in some circumstances, but I urge you to explore healing your own tissue, with their help, if it is all possible.
Be careful in picking a regenerative orthopedist as many insufficiently trained practitioners have jumped on the bandwagon to make a quick buck. This practice has trained other physicians around the country. Also, know as much about your condition and the cause of your pain as you possibly can before you see your orthopedist because they are extremely busy. Don’t expect much bedside manner. I suspect, in my case, we might have tried an epidural instead of a facet injection first if I had a long talk with my primary pain management doctor prior to treatment at the Centeno Schultz clinic. After five years, I suspect he knew it was nerve pain rather than facet pain. But I never specifically asked anyone who had been treating me for years. That was a mistake. You have to be your own advocate. That would’ve cut almost a year of trial and error and pain and cost out of my treatment. And, especially if you are a woman, don’t accept any verdict that it is “all in your head”. Pain is a complex phenomenon involving your entire nervous system, including your brain, and the place of your initial injury, disease or other source of pain. Learn about pain. You will find recent research fascinating.
At the very least, do yourself a favor and read their downloadable book.”
We’re happy that Heidi is doing well and so thankful that yet another patient realizes what we doctors have, that platelet lysate for spine conditions is a game changer!
The post New Treatment for Neck Pain: Platelet Lysate and Heidi’s Journey appeared first on Regenexx®.